Streamline Your Emergency Department Billing with MedsIT Nexus Expert Services
Emergency Department (ED) billing isn’t standard billing — it’s complex, high-stakes, and demands precision. From hospital facility charges for nursing care, supplies, and trauma activation to physician claims for E/M services, procedures, and critical care, every detail counts. Our expert team navigates the maze of UB-04 forms, CPT codes, revenue codes, and compliance rules like EMTALA and the No Surprise Billing Act. Whether you’re billing for a hospital ED or an emergency physician group, we help you capture every dollar, cut denials, and boost revenue. Let’s simplify your ED billing today.
Go to Pricing
Accomplish Rapid Growth
Billing complications slow down operational efficiency. Get rid of the hassle with our qualified billing experts and boost your revenue
Get a QuoteHIPAA
Compliant
Ensure
Accuracy
Client
Satisfaction
Collection
Ratio
Revenue
Increase
First
Pass Rate
Stop Losing Revenue with MedsIT Nexus Emergency Department and Physician Billing Professionals
Many billing teams get stuck here, & revenue slips through the cracks. Emergency Department billing covers facility fees charged by the hospital for room usage, nursing care, equipment, & supplies. This is billed on UB-04 forms using revenue codes & APCs. On the other hand, emergency physician billing is separate, covering the doctor's time, decision-making, and procedures. Physicians bill using CPT codes on CMS-1500 forms. Both streams must work in sync, following distinct rules, coding systems, & reimbursement models. Our team ensures you capture every dollar from both facility & physician claims, without errors or delays.

Emergency Department Billing & Coding
Emergency Department (ED) Billing demands a specialized level of expertise that goes beyond standard outpatient billing. Unlike professional billing, where each service is coded and billed individually, ED facility billing often involves bundled payments through Ambulatory Payment Classifications (APCs). Successfully managing these complex claims requires deep knowledge
and hands-on experience in.
APC Bundling Rules
With a perfect understanding of CMS and APC, we ensure accurate grouping and coding of bundled services, like ED services, nursing care, room charges, and diagnostics and supplies into bundled payment levels. Our team ensures the correct assignment of ED visit levels (1-5) to maximize reimbursement while maintaining compliance.
Revenue Code Mastery
Skilled billers can use precise revenue codes (e.g., 0450 for general ED services, 0300 for labs, 0320 for radiology) to capture all reimbursable services within facility claims. Misuse can trigger denials or underpayments.
Institutional Claims Processing Specialists
Unlike professional billing, our team processes institutional claims on the UB-04 (837I) format, ensuring facility resources are billed through the correct pathways and reimbursement flows efficiently.
Payer & OPPS Compliance Experts
We navigate payer-specific bundling rules and align your billing with CMS OPPS regulations — preventing revenue loss and maximizing reimbursement across Medicare, Medicaid, and commercial plans under the latest federal and payer guidelines.
Compliance & Audit Readiness
Given the scrutiny around upcoding or misleveling ED visits, experienced billing companies maintain robust compliance checks and audit protocols to ensure accurate, defensible claims
Why Experience Matters
Without experts handling, ED billing can lead to:
Downcoded claims due to improper
facility-level assignment.
Missed revenue from imcomplete
charge capture
Denied ancillary services that could
have been billed separately
Payer audits due to billing
discrepancies
MedsIT Nexus deeply understands Hospital Outpatient Billing Services, ensuring every ED claim aligns with institutional billing standards, which helps you get paid faster.
Expert Emergency Room Physician Billing Services
Emergency room physician billing is a specialized process beyond standard medical billing. Unlike facility billing, it focuses on capturing ER doctors' professional services — from complex patient evaluations to life-saving procedures. Each claim requires precise coding, correct modifier application, and strict compliance with payer rules to avoid denials and secure full reimbursement. At MedsIT Nexus, we bring the following expertise, experience, and attention to detail needed to streamline your emergency physician billing, protect your revenue, and keep your practice audit-ready.

Mastery of E/M Coding & MDM Rules
Our billing specialists are experts in assigning precise Emergency Department
E/M codes (99281–99285) based on Medical Decision-Making (MDM). We ensure your
claims reflect the full complexity of care, maximizing
revenue while maintaining
compliance.
Precision in Procedural Coding
From laceration repairs to fracture care, our team bills each procedure separately using the correct CPT codes. This unbundled approach captures every service performed, preventing revenue leakage.
Modifiers Application Experts
We skillfully apply critical modifiers like -25 and -57, distinguishing procedures from E/M services and defending your claims against denials and audits
Global Surgical Package Expertise
Our team navigates the global surgical package rules specific to ER physician procedures, ensuring accurate billing for both initial treatment and bundled post-procedure care.
Compliance & Medical Necessity Defense
With deep payer knowledge, we help physicians document in line with medical necessity rules, avoiding downcoding and protecting against payer audits.
Professional Claims Processing Specialists
Unlike institutional billing, our team processes professional claims on the CMS-1500 (837P) format, ensuring that your physician services are billed accurately, modifiers are applied correctly, and reimbursements flow smoothly
through payer systems designed
for professional providers
Why Experience Matters in ER Physician Billing
Without experienced handling, ER physicians' claims face risks like:
Downcoded E/M levels
Denied procedures due to missing
modifiers
Credentialing delays blocking
payment
Payer audits triggered by
coding discrepancies
At MedsIT Nexus, we bring years of frontline experience handling emergency physician billing complexities, ensuring your practice gets paid fully, fast, and compliantly.
Emergency Department Revenue Cycle Management Services
Specialized RCM Tailored for the Chaos, Compliance, and Critical Nature of Emergency Care
In the emergency department, seconds matter — not only for patient outcomes but also for financial performance. MedsIT Nexus brings unmatched precision to Emergency Department Revenue Cycle Management (ED RCM), purpose-built to support trauma-informed workflows, unscheduled care patterns, and high-stakes billing environments. Here’s how we redefine each stage of the ED financial lifecycle:
In the emergency department, seconds matter — not only for patient outcomes but also for financial performance. MedsIT Nexus brings unmatched precision to Emergency Department Revenue Cycle Management (ED RCM), purpose-built to support trauma-informed workflows, unscheduled care patterns, and high-stakes billing environments. Here’s how we redefine each stage of the ED financial lifecycle
In the emergency department, seconds matter — not only for patient outcomes but also for financial performance. MedsIT Nexus brings unmatched precision to Emergency Department Revenue Cycle Management (ED RCM), purpose-built to support trauma-informed workflows, unscheduled care patterns, and high-stakes billing environments. Here’s how we redefine each stage of the ED financial lifecycle
In the emergency department, seconds matter — not only for patient outcomes but also for financial performance. MedsIT Nexus brings unmatched precision to Emergency Department Revenue Cycle Management (ED RCM), purpose-built to support trauma-informed workflows, unscheduled care patterns, and high-stakes billing environments. Here’s how we redefine each stage of the ED financial lifecycle
In the emergency department, seconds matter — not only for patient outcomes but also for financial performance. MedsIT Nexus brings unmatched precision to Emergency Department Revenue Cycle Management (ED RCM), purpose-built to support trauma-informed workflows, unscheduled care patterns, and high-stakes billing environments. Here’s how we redefine each stage of the ED financial lifecycle
In the emergency department, seconds matter — not only for patient outcomes but also for financial performance. MedsIT Nexus brings unmatched precision to Emergency Department Revenue Cycle Management (ED RCM), purpose-built to support trauma-informed workflows, unscheduled care patterns, and high-stakes billing environments. Here’s how we redefine each stage of the ED financial lifecycle
In the emergency department, seconds matter — not only for patient outcomes but also for financial performance. MedsIT Nexus brings unmatched precision to Emergency Department Revenue Cycle Management (ED RCM), purpose-built to support trauma-informed workflows, unscheduled care patterns, and high-stakes billing environments. Here’s how we redefine each stage of the ED financial lifecycle


-
Medical Billing Audit for Emergency Departments
Catch What Most Miss in Split Billing & Modifier Use
Emergency room cases often involve multiple providers, urgent diagnostics, and split/shared services. Our audits detect inconsistencies in critical care modifiers (like -25, -76), improper ED level coding (99281–99285), and physician/PA split billing errors that can trigger payer denials or audits. We proactively close revenue gaps before payers find them. -
Emergency Medical Credentialing Enrollment
Fast-Track Onboarding for ED Physicians & Mid-Level Providers
Emergency physicians and PAs often work across multiple hospitals or staffing groups, requiring complex credentialing pathways. We expedite NPI enrollment, hospital privileging, payer contracting, and CAQH maintenance, with special attention to locum tenens and night-shift rotation scenarios unique to ED settings. -
Emergency Insurance Verification
Real-Time, No-Margin-for-Error Coverage Checks
Coverage determination in the ED must happen quickly, often while the patient is already under care. Our real-time insurance verification solutions ensure accurate identification of payer status, benefit limits, and authorization requirements even under emergent conditions. We reduce denials from front-end failures. -
Emergency Medical Coding Services
Code with Confidence in Chaos
ED coding isn’t just about 99285. Our certified emergency coders can extract revenue from chaos without compliance risks, from laceration repairs and critical care time capture to ECG interpretation and procedural bundling. We maintain accuracy across ICD-10-CM, CPT®, and HCPCS within hospital-based ED environments. -
Emergency Accounts Receivable (A/R) Management
Reduce A/R Days for the Fastest-Moving Department in the Hospital
The ED doesn’t pause — and neither should your cash flow. We actively monitor claim status, chase down unpaid encounters, and resolve denials tied to ED-specific complications such as incorrect POS codes or disputed medical necessity. Our A/R team is tuned for high-volume, 24/7 departments. -
Emergency Department Denial Management Services
Fight Denials Specific to the Fastest-Paced Environment in Healthcare
In the emergency department, even minor billing missteps can snowball into major revenue loss, especially when dealing with 24/7 services, complex coding levels, or multi-provider care. MedsIT Nexus applies deep expertise in emergency-specific denial patterns to reduce rework, resubmit quickly, and protect your bottom line.
Real-Time Charge Capture in the ED
From Action to Reimbursement Without Delay
In the high-pressure environment of an Emergency Department, every moment counts — not just clinically, but financially. Real-time charge capture ensures that all billable services — from triage to discharge — are recorded instantly as care is delivered.
Eliminates Missed Charges
Captures procedures, supplies, & interventions that might otherwise be overlooked in retrospective documentation.
Enhances Coding Accuracy
Supports coders with precise, time-stamped service data, reducing errors and denials.
Speeds Up Billing
Reduces lag between care delivery and claim submission, accelerating revenue cycles.
Improves Compliance
Aligns with CMS and payer requirements by linking real-time documentation to medical necessity.
At MedsIT Nexus, we help emergency departments implement seamless real-time charge capture systems — integrating EHRs, clinical workflows, and billing engines for maximum revenue integrity
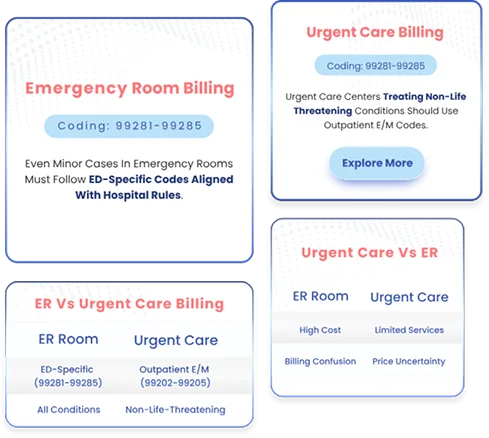
Avoid Costly Audit Triggers, Separating ER & Urgent Care Billing
Payers closely audit claims to ensure that Emergency Room visits and Urgent Care services are billed under the correct coding framework. Urgent Care centers, which treat non-life-threatening conditions, should be billed using outpatient E/M codes (99202-99205) — a process distinct from Emergency Room billing, where even minor cases must follow ED-specific codes (99281-99285) aligned with hospital rules. Our billing experts help safeguard your revenue by properly separating ER and Urgent Care claims, ensuring compliance while optimizing Urgent Care Billing Services that truly differ from ER billing, reducing denials, and preventing costly audits.
Emergency Medical Specialists Billing Services
In the high-acuity environment of the Emergency Department, care extends far beyond the attending ER physician. From trauma surgeons and neurologists to physician assistants (PAs) working across multiple specialties, the ED is a coordinated frontline of medical expertise. Yet, billing for these diverse emergency medical specialists — especially PA-provided care under supervising specialists — requires a refined understanding of coding, scope of practice, and payer-specific compliance. That’s where MedsIT Nexus delivers unmatched value. We bring deep domain expertise in billing for on-call and interdisciplinary emergency specialists, including PAs who extend specialist care, ensuring that every service is accurately captured and reimbursed under professional billing standards.
Subspecialty-Specific Coding Mastery
Our certified coders are fluent in procedural and consultative billing for
Trauma Surgery
Critical Care Medicine
Anesthesiology
Emergency Cardiology
Physician Assistant
Neuro & Stroke Response
Orthopedics & Fracture Management
We ensure each CPT code, NPI attribution, and supervisory billing rule is applied correctly, whether services are provided directly by the specialist or incident-to care by a PA.
Integrated Specialist & PA Documentation
In fast-paced ER cases, PAs often provide initial or follow-up care, conduct procedures, or assist in specialty-driven interventions. We align specialist and PA documentation to ensure non-overlapping, billable claims with correct modifiers and supervision indicators.
Modifier & Supervisory Billing Compliance
From NPP modifiers to appropriate use of AS (Physician Assistant, Surgical Assistant), our billing team ensures full compliance with:
-
Medicare’s split/shared visit rules
-
Incident-to billing restrictions
-
State scope-of-practice variations
-
Commercial PA reimbursement policies
Precision in Split-Claim Scenarios
We handle the complexity of multi-provider and PA-inclusive billing, tracking distinct time segments, documentation chains, and shared care models. We ensure each provider’s contribution is billable and not denied due to duplication.
CMS-1500 Professional Claim Expertise
All emergency medical specialties and PA services are billed on the CMS-1500 form. We ensure clean coding across CPT, HCPCS, and diagnosis capture accurately linking procedures, consults, and PA-assisted care to maximize payment and avoid underbilling.


Why MedsIT Nexus?
At MedsIT Nexus, we specialize in billing demands for emergency department specialists and their physician assistants. Whether services are direct, collaborative, or supervised, we ensure every dollar tied to your expertise is coded correctly, defended, and collected.
Your emergency care is urgent your reimbursement shouldn't wait. Let MedsIT Nexus help you protect revenue, ensure compliance, and secure payment for every provider in the emergency room team.
Emergency Medical Services Billing Precision
In the high-acuity environment of the Emergency Department, care extends far beyond the attending ER physician. From trauma surgeons and neurologists to physician assistants (PAs) working across multiple specialties, the ED is a coordinated frontline of medical expertise. Yet, billing for these diverse emergency medical specialists — especially PA-provided care under supervising specialists — requires a refined understanding of coding, scope of practice, and payer-specific compliance. That’s where MedsIT Nexus delivers unmatched value with Expertise emergency specialists and PAs billing, ensuring accurate & compliant reimbursement.

CMS Rules, Your Revenue
Emergency Department Billing Done Right
Navigate every guideline to unlock full reimbursement. Stay audit-proof
At MedsIT Nexus, we don’t just process claims — we protect your revenue by aligning every Emergency Department charge with CMS compliance rules. Our team decodes federal billing logic so you can focus on clinical excellence
OPPS Compliance
We align your ED billing with CMS’s Outpatient Prospective Payment System (OPPS) to ensure you receive accurate, APC-based reimbursements. There will be no missed revenue and no outdated codes.
Code 99281–99285
Our experts select the correct ED E/M level based on resource intensity, not time or documentation templates. We follow CMS facility-level coding logic to the letter.
Documentation
From triage notes to diagnostics, we ensure your documentation clearly supports every code, protecting you from audits while boosting clean claim rates.
Add-On Services
We identify and bill separately for minor procedures, infusions, or imaging when CMS allows it. You get what you’ve earned; there is nothing left on the table.
Modifier Mastery
Our coders apply Modifier 25, 59, XE, XS, and others with precision, ensuring your ED services aren’t unfairly bundled or denied.
Billing Components
ED facility and professional claims require distinct strategies. We know the difference and bill them right, so there is no overlap or compliance flags.
Why This Matters
Emergency Departments operate in real-time chaos. That’s why your billing demands real-time expertise. With MedsIT Nexus, your claims stay compliant, complete, and confidently coded under CMS rules.
Ready to Take Control of Your Emergency Department Revenue?
Let our certified ED billing experts ensure compliance, clarity, and collections
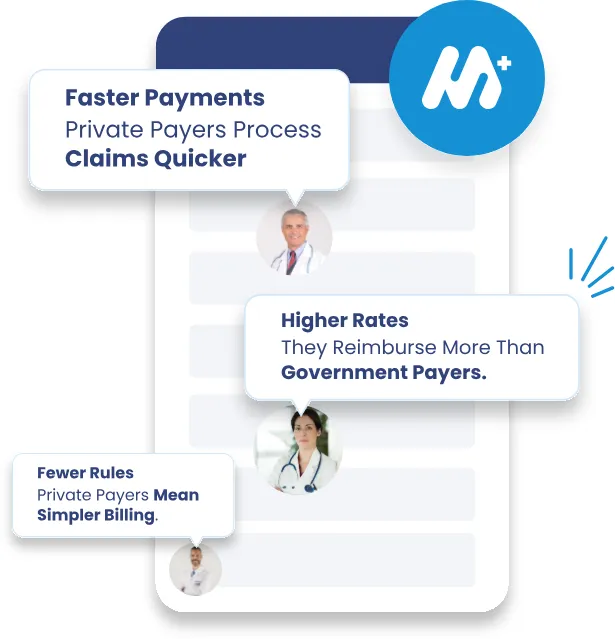
Private vs Government Payers: Two Paths, One ER
Emergency Room Billing isn’t one-size-fits-all, especially when payers play by different rules.
Private insurers demand pre-authorizations, apply proprietary coding edits, & often delay payments through internal audits. In contrast, Medicare & Medicaid Emergency Department reimbursement is governed by strict CMS protocols — including OPPS (Outpatient Prospective Payment System), EMTALA mandates, & predefined bundling logic — yet requires expert interpretation to avoid underpayments or compliance penalties. At MedsIT Nexus, we master both lanes. Whether it's a commercial claim or a government-backed one, we optimize every ER submission to align with each payer's rulebook, accelerating your cash flow and safeguarding your compliance.
Your ER saves lives. we save your revenue!
ED Billing Software & EHR Integration
Synchronize Care with Reimbursement—In Real Time
Fragmented systems in the Emergency Department mean fragmented revenue. That’s why seamless integration between your ED billing software and Electronic Health Records (EHR) is non-negotiable. At MedsIT Nexus, we ensure your billing engine talks directly to your clinical systems without friction or lag.
Let's Streamline your Billing
What You Gain
Real-Time Data SyncCharges, documentation, and procedures flow instantly into billing pipelines.
Code-Ready DocumentationAuto-mapped CPT/HCPCS codes from physician notes reduce coder guesswork.
Reduced Claim ErrorsIntegrated workflows minimize missed modifiers, incomplete forms, & compliance risks.
Faster Claim SubmissionStreamlined processing shortens billing cycles & improves cash flow.
With our tailored ED billing & EHR integration strategies, you don’t just capture care—you convert it into compliant, timely reimbursement with zero data loss.
Specialized Emergency Room Billing Expertise
Mastering the Most Complex Scenarios in the ED
Not all emergency cases are created equal, and neither are their billing requirements. At MedsIT Nexus, our specialized medical billers and coders are trained to handle high-acuity, high-complexity emergency room services that often fall outside standard billing protocols. We turn critical care chaos into revenue clarity.
Trauma Billing in ED
When the trauma team is activated, documentation & billing must be immediate, accurate, & compliant with CMS & commercial trauma guidelines. Our experts ensure correct Level I–V trauma activation fees are captured, documented, & billed to avoid costly denials or underpayments.
Emergency Surgical Procedures & Billing
Emergency surgeries require precise CPT coding, correct modifier use, and coordination with inpatient or outpatient status. MedsIT Nexus ensures bundled surgical codes are clean, timely, and compliant with payer-specific edits so surgeons get paid, even in urgent cases.
Emergency Room Anesthesia Billing
From procedural sedation to emergent intubation, our anesthesia billing specialists accurately capture time units, ASA modifiers, and concurrency rules. We coordinate closely with anesthesiology documentation in real-time to reflect critical care involvement.
Telemedicine in Emergency Settings
Tele-ED is growing fast, but billing errors are also increasing. Our team understands the latest CMS telehealth policies, place of service codes, and emergency tele-triage billing workflows. We ensure that virtual care doesn’t result in virtual revenue loss.
Pediatric Emergency Billing
Pediatric encounters demand more than general ED coding—they require age-specific documentation, growth-based medication coding, and specialized modifiers. Our coders are trained in pediatric guidelines and CPT nuances to maximize payment for even the tiniest patients.
Behavioral Health Encounters in ED
When behavioral health crises occur in the ED, billing can be tricky—mental health CPTs, observation status, and facility-based evaluation codes all apply. MedsIT Nexus ensures that your reimbursement reflects the intensity and duration of care delivered.
Why MedsIT Nexus?
Because your Emergency Room never sleeps—and neither does our expertise.
We don’t just process claims; we specialize in the unpredictable, urgent, and high-stakes world of ER billing. With MedsIT Nexus, every specialty is accounted for, every scenario optimized, and every code justified.
Secure reimbursement & Elevate revenue with MedsIT Nexus RCM Partnership.
Hospital Owned ED vs Free Standing ED Billing
Different Structures One Expert Billing Partner MedsIT Nexus
Not all Emergency Departments are built the same, & neither are their billing complexities. At MedsIT Nexus, our expert billing & coding professionals underst & the critical distinctions between Hospital-Owned Emergency Departments (HOPDs) & Free-Standing Emergency Departments (FSEDs) & how these structural differences directly impact how claims are coded, billed, & reimbursed.
Why This Matters
Misclassification between FSED and HOPD billing structures can result in claim denials, compliance risk, & revenue loss. Our team decodes your organizational status at the NPI level, ensuring every claim reflects the correct place of service, revenue codes, & fee schedules.
Let us Align Your Billing with Your ED’s True Identity
Facility-based. CMS-regulated. OPPS-driven. We ensure accurate institutional billing under CMS’s Outpatient Prospective Payment System (OPPS), integrating UB-04 claims with physician CMS-1500 submissions, while accounting for cost-based reporting, trauma activation, & facility-level E/M coding.
Our Expertise in Action
-
Correct use of POS 19 vs. POS 22
-
Split billing for facility + professional services
-
Modifier usage for off-campus HOPDs
-
Navigating Medicare’s Site Neutral Payment Rules
Our billing team navigates complex state licensure rules and payer-specific recognition of free-standing EDs. Whether it’s a non-provider-based FSED or a satellite of a hospital, we tailor claims to reflect appropriate service location modifiers, global vs. split billing, and nuanced documentation.
Our Expertise in Action
-
Correct use of POS 19 vs. POS 22
-
Split billing for facility + professional services
-
Modifier usage for off-campus HOPDs
-
Navigating Medicare’s Site Neutral Payment Rules
ED Billing in Rural vs. Urban Hospitals
Different Settings, Distinct Billing Realities, Same Need for Expertise.
Emergency Department billing isn’t one-size-fits-all. Rural and urban hospitals face vastly different reimbursement landscapes, and at MedsIT Nexus, we tailor our billing strategies to fit each environment.
Schedule a Discovery Call Book Now
Rural Hospital ED Billing
Rural hospitals often operate under Critical Access Hospital (CAH) designation, which shifts billing from standard APCs to cost-based reimbursement models. That means your billing team must:
Apply Method II billing when appropriate
Navigate split billing for professional and technical components
Maximize payment through accurate cost reporting
Ensure proper Medicare Condition Code use
Urban Hospital ED Billing
Urban EDs deal with greater patient flow, more diverse payers, and frequent overlap between trauma teams, specialists, and outpatient services. Our billing solutions for urban facilities include:
Accurate facility-level E/M leveling (99281–99285)
Payer-specific edits for commercial and Medicaid MCOs
Integration of multiple provider specialties
Modifier usage to separate bundled services
We understand the rural reality, where every dollar matters and payer rules demand precision.
Why It Matters
The differences in rural vs. urban ED billing aren’t just operational but financial lifelines. Misapplied rules or one-size-fits-all billing approaches can lead to revenue loss or compliance risks.


State-wise ED Reimbursement Variations
Your Location Determines Your Compensation — We Make Sure You Don’t Miss a Cent
Emergency department billing isn’t just federally regulated — state-specific Medicaid rules shape it, managed care plans, & reimbursement formulas. That’s why your billing partner needs more than a national strategy — you need localized precision
Every State, Different Rules
From California's Medi-Cal reimbursement caps to Texas Medicaid’s Level-of-Service restrictions, each state applies its own ED visit thresholds, modifiers, and prior authorization requirements — even for emergency services.
At MedsIT Nexus, we decode:
-
Unique crossover billing rules
-
State Medicaid fee schedules & limitations
-
Level 1–5 ED visit restrictions & documentation mandatess
-
State-specific Managed Care Organization (MCO) edits & denials
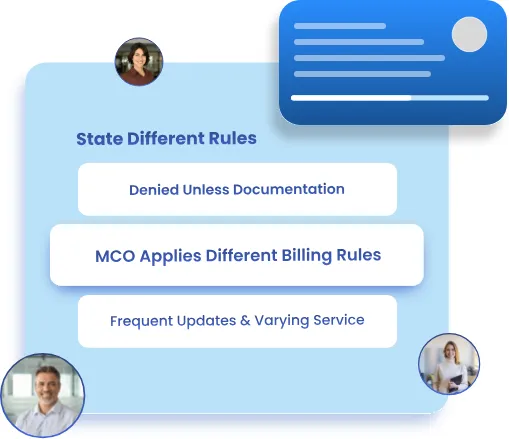

Why This Impacts Your Revenue
Ignoring these state-based rules results in down-coding, denials, and delayed reimbursements. Our state-optimized RCM protocols ensure that every emergency claim:
-
Is coded per state-accepted E/M leveling
-
Meets the proper medical necessity documentation
-
Passes through the correct MCO adjudication process
-
Avoids frequent compliance pitfalls in high-scrutiny states
Local Focus National Compliance
Whether your Emergency Department operates in New York, Florida, Illinois, or rural Montana, we bring state-aware billing expertise to every claim. At MedsIT Nexus, we proactively track annual changes in state reimbursement trends, update payer rules, and align your ED billing workflows to maximize revenue with zero guesswork.
Stay Reimbursed, Not Rejected
Your state shouldn’t be a barrier to fair payment. Let MedsIT Nexus keep your Emergency Department billing compliant, accurate, and paid — wherever you practice.
Emergency Group Practice Billing Vs Independent Contractor Billing
Two Billing Models. One Common Goal: Get Paid Precisely for ER Expertise.
In the high-stakes emergency medicine environment, billing structures vary by patient or payer and how emergency physicians are employed. Whether operating under a Group Practice Model or as Independent Contractors, revenue cycle strategies must be carefully tailored to avoid compliance risks and maximize collections.
Why It Matters to Billing Success
MedsIT Nexus brings tailored billing workflows for each structure. Whether you're a group entity with multiple hospital contracts or an independent ER physician managing your own books, we:
Emergency physicians employed within hospital-based group practices or larger contracted teams typically benefit from centralized billing processes, shared credentialing, & unified payer agreements. This model offers streamlined workflows & consistent coding practices, especially vital in high-volume ER settings. Much like the operational dynamics found in Small Practice Billing, group billing environments depend on shared administrative structures to reduce friction & enhance claim accuracy. However, they scale these efficiencies across multiple providers and ER shifts.
Key Advantages
-
Integrated revenue cycle workflows
-
Centralized NPI/TIN under one entity
-
Unified documentation and coding protocols
-
Less administrative burden on individual providers
On the other hand, independent emergency physicians — including locum tenens and self-employed ER specialists — manage their billing independently or through niche billing partners. These providers often operate similarly to Private Practice Billing, where greater autonomy requires tighter control over claim submission, credentialing, and payer negotiations. This model presents unique challenges, especially around compliance with out-of-network billing laws and managing variable reimbursement patterns.
Key Considerations:
-
Separate NPIs or Tax IDs
-
Independent payer contracts
-
Higher exposure to denials and audit risk
-
Need for precise documentation and claim tracking
No Surprises Act: Reshaping Emergency Department Billing Standards
Your Location Determines Your Compensation — We Make Sure You Don’t Miss a Cent
The No Surprises Act (NSA) — enacted in January 2022 — introduced sweeping reforms to protect patients from unexpected out-of-network bills after emergency care. But behind the scenes, this legislation has fundamentally altered ED billing workflows, payer negotiations, and provider reimbursement.
What It Means for ED Providers
Emergency departments are required to deliver immediate care without regard to insurance networks, uniquely affecting them by this law. Under NSA:
-
Out-of-network ED providers can no longer balance bill patients beyond in-network cost-sharing
-
Payment disputes are now handled through a federal independent dispute resolution (IDR) process
-
Good faith estimates (GFEs) and notice & consent protocols apply in post-emergency or follow-up care
-
Commercial payers must reimburse based on median in-network rates, not billed charges
Impact on ED Billing Operations
At MedsIT Nexus, we’ve helped emergency departments and billing teams rapidly adapt to the NSA mandates by
-
Implementing NSA-compliant claim workflows
-
Auditing payer adjudication for underpaid out-of-network claims
-
Supporting IDR submissions when payers offer below-median benchmarks
-
Ensuring proper coding and documentation to meet emergency medical condition standards
-
Preventing audit exposure related to improper balance billing or notice violations
Reimbursement Pressure & Operational Adjustments
While patient protections are commendable, the NSA has created revenue uncertainty for many hospital-based emergency physicians & independent ED groups, especially in rural or underserved areas with limited in-network coverage.
-
Avoid underpayment on emergency visits (99281–99285)
-
Optimize revenue via compliant, payer-specific workflows
-
Navigate state vs. federal NSA alignment in hybridregulated markets


Stay Compliant. Stay Paid Emergency medicine doesn’t pause and neither do we.
MedsIT Nexus brings NSA-ready billing strategies that ensure compliance without compromising revenue. From documentation to dispute resolution, we keep your ED billing secure and responsive in this evolving regulatory landscape.
Learn More About Our Emergency Department Billing Services
Transitional Billing Complexities in Emergency Care
Where Patient Status Meets Reimbursement Challenges
In the Emergency Department, patients don't always follow a linear path—what starts as an outpatient evaluation can escalate into inpatient admission within hours. This shift triggers a seismic change in how services are billed. ED services initially coded under outpatient Evaluation & Management (E/M) codes (99281–99285) may need rebundling or split billing when inpatient status is assigned. Failure to reclassify correctly can result in underpayments, compliance issues, or claim rejections. At MedsIT Nexus, our billing experts stay ahead of these pivot points, ensuring accurate claim sequencing and status alignment to capture every dollar earned—legally and ethically.
Outpatient-to-Inpatient Transition Billing
From Observation to Admission—Handled Without Gaps
When emergency patients are placed under observation status before being admitted, this creates a billing gray zone. Observation services billed with codes like G0378 (hourly observation) may overlap with inpatient care. The key? Knowing when to split claims and when to roll over charges. Our team understands the nuances of Medicare's 2-Midnight Rule and private payer timelines, ensuring compliant transitions that don’t shortchange your revenue.
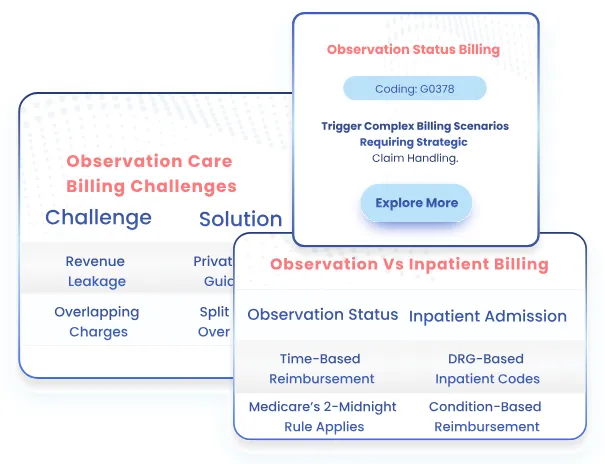
Inpatient-to-Outpatient Return Visits
Same-Day Discharges and ED Readmissions Done Right
What happens when a recently discharged inpatient returns to the ED on the same day or within 72 hours? Whether it’s a related diagnosis or an unrelated event, it has massive billing implications. CMS may bundle these services into the prior inpatient DRG unless you know how to clearly document medical necessity and code modifiers. MedsIT Nexus ensures your claims don't fall into these audit traps with ironclad documentation alignment and modifier precision.
Modifier Mastery in Status Shifts
The Power of -25, -59, and -PO
Status transitions demand skilled use of billing modifiers.
For example:
-
Modifier -25 justifies significant E/M service beyond the procedure.
-
Modifier -59 identifies distinct procedural services in same-day ED-to-OR scenarios.
-
Modifier -PO flags services under CMS’s site-neutral payment policies.
Each modifier requires careful clinical documentation & timing logic. Our coders don't just add modifiers—they back them with airtight documentation that survives any payer review.
Observation Services vs. Short-Stay Admissions
When Minutes Matter, So Does Billing Precision
In the fast-paced environment of Emergency Departments, distinguishing between observation status and short-stay inpatient admissions isn’t just clinical—it’s a revenue-critical decision. At MedsIT Nexus, we bring deep experience in helping hospitals navigate this gray zone where patient status, length of stay, and clinical intent intersect with the CMS Two-Midnight Rule, utilization review, and DRG assignmen.
Why It Matters:
Observation stays fall under the Outpatient Prospective Payment System (OPPS), while short-stay admissions trigger the Inpatient Prospective Payment System (IPPS) reimbursements. A misclassification can lead to denied claims, compliance audits, or underpayments.
Our Expertise Covers:
-
Proper use of Condition Code 44
-
Billing based on physician order compliance
-
Documentation that defends medical necessity
-
Revenue optimization between C-APCs and MS-DRGs
We ensure that your facility captures the right payment pathway while remaining fully compliant with payer rules and CMS audits.

Patient Arrival at the ER from the Ambulance
Where Prehospital Care Meets Emergency Room Precision
The moment a patient arrives at your Emergency Room via ambulance, the billing journey splits into two distinct yet interconnected tracks: EMS billing and Emergency Department billing. This critical transition requires not only clinical coordination but also meticulous documentation and coding accuracy. At MedsIT Nexus, we specialize in bridging this care-to-claim gap.
Why It Matters:
Ambulance services bill separately using HCPCS Level II codes (A0425–A0436) under Medicare Part B, while ER services begin with ED E/M codes (99281 - 99285). The patient's condition, transport justification, and arrival time all influence billing outcomes.
Our Expertise Includes:
-
Seamless data transfer from EMS to ED
-
Ensuring modifiers are applied correctly
-
Proper linkage of ambulance transport claims with ER medical records
-
Aligning EMS trip reports with medical necessity documentation for ER visits
We ensure every code, mile, and minute is captured so your revenue doesn’t slip through the cracks during this high-stakes handoff.
With MedsIT Nexus, your emergency billing cycle begins before the ER doors open, because we know reimbursement starts at the curb.
Case Studies: How MedsIT Nexus Helped USA Hospitals Cut Costs, boost Reimbursements, & Enhanced RCM
Ready to Unlock 30% More in ED Reimbursements?
From rural facilities to Level 1 trauma centers, hospitals nationwide have already transformed their emergency department revenue with MedsIT Nexus. Whether you're battling downcoding, facing EMS billing gaps, or navigating complex APC logic, we bring proven, specialty-driven solutions that work.
Outsource ER Billing to MedsIT Nexus—Get Paid
Faster, With Fewer Headaches
Emergency Room billing is complex, time-sensitive, and high-volume. One mistake delays reimbursement. One missed code means lost revenue That’s why hospitals and urgent care centers choose MedsIT Nexus.
Accurate Coding, Every Time
Our certified coders understand the nuances of ER claims—from trauma level charges to modifiers and split billing. We minimize denials from day one.
Faster Claims, Faster Cash Flow
We process ER claims within 24 hours. Our clean claim rate exceeds 96%, which means less time chasing unpaid bills and more revenue in your hands.
Compliance-First Approach
Emergency departments face intense regulatory scrutiny. We stay ahead of CMS changes and payer rules so you don’t have to.
Transparent Reporting
Track reimbursements, denial trends, and productivity in real time. No guesswork—just clear data.
Scalable Support
From rural hospitals to high-volume urban EDs, our team scales to meet your needs without sacrificing accuracy or turnaround time.
MedsIT Nexus is not a generic billing firm. We specialize in hospital-based services like Emergency Room billing—where accuracy, speed, and compliance matter most.
Schedule a quick discovery call. We’ll show you exactly where you’re losing revenue—and how we’ll fix it.
Get a Free Revenue Cycle Assessment Today
our revenue cycle experts Identify gaps & unlock higher profitability
Our services are trusted by 2000+ providers

Schedule a Free Demo
Sign up and book a free service demo
Free Demo

Get Started Today
Connect with RCM expert for free billing audit
See pricing packages


 Medical Billing Audit for Emergency Departments
Medical Billing Audit for Emergency Departments
 Emergency Medical Credentialing Enrollment
Emergency Medical Credentialing Enrollment
 Emergency Insurance Verification
Emergency Insurance Verification
 Emergency Medical Coding Services
Emergency Medical Coding Services
 Emergency Accounts Receivable (A/R) Management
Emergency Accounts Receivable (A/R) Management
 Emergency Department Denial Management Services
Emergency Department Denial Management Services

