What is Hierarchical Condition Category Coding: Why it’s Important to Healthcare Providers?
In the ever-evolving healthcare landscape, accurate and efficient medical billing has emerged as a crucial component for healthcare providers and insurance companies. Among the various coding systems used in the industry, Hierarchical Condition Category (HCC) coding has gained prominence for its ability to capture the complexity of patient conditions and drive appropriate reimbursement. However, the intricate nature of HCC coding demands specialized expertise and meticulous attention to detail. This is where professional medical billing companies play a pivotal role, offering a comprehensive range of services to ensure accurate HCC coding and maximize revenue for healthcare organizations. In this article, we will delve into the intricacies of HCC coding and explore its importance.
Hierarchical Condition Category Coding
Before knowing about HCC coding, it is necessary to understand what is HCC? Hierarchical Condition Categories (HCCs) are a set of diagnosis codes grouped into categories that capture patients’ clinical conditions and predict their future healthcare costs. HCCs are organized into multiple levels, with higher-level categories representing broader disease states (e.g., diabetes or heart failure) and lower-level categories delving into more specific manifestations or complications (e.g., diabetic neuropathy or congestive heart failure with systolic dysfunction). Each HCC category is assigned a numerical risk coefficient, reflecting the relative expected costs associated with managing patients in that category.
HCC Coding Defined
Now you understand HCC, and it is better to know what is hierarchical condition category coding. HCC
coding, initiated in 2004, is a risk-adjustment model used by government-sponsored healthcare programs,
such as Medicare Advantage and the Affordable Care Act, to accurately estimate healthcare costs and
reimburse providers accordingly. Hierarchical Condition Categories (HCCs) Coding Model operates on a
hierarchical structure, grouping related diagnoses into categories that reflect the expected cost and
resource utilization for managing a patient’s health conditions.
The primary purpose of HCC coding is to capture the severity of a patient’s health conditions and
predict the anticipated cost of their care over time.
Major Health Conditions For HCC Coding
- Prostate cancer
- Breast cancer
- Bipolar disorder
- Diabetes
- Colorectal kidney
- Colorectal breast
- Rheumatoid arthritis
- Congestive heart failure
- Pulmonary diseases
- Specified heart arrhythmias
- Endocrine disorders
- Stroke
Processing HCC Coding
The submission of diagnoses for HCC coding by physicians’ coders does not directly go to the government;
instead, this task is carried out by the system’s health plan involved. According to AAPC, the following
steps are followed in this process.
1st step: The health plan requests medical records from healthcare providers for
the HCC coder to review.
2nd step: HCC coders review the medical records to extract supported
conditions/ICD-10-CM codes that map to an HCC.
3rd step: HCC coders insert the extracted codes in the company’s data repository.
4th step: Quality assurance staff reviews abstracted HCC-relevant ICD-10-CM codes
to ensure accuracy.
5th step: The company submits abstracted diagnosis codes to CMS or HHS in the
repository.
6th step: CMS or HHS uses the submitted ICD-10-CM codes to calculate the risk
score of each enrolee and send payment to the health plan.
HCC Coding Classifications
Concurrent HCC Coding
Concurrent HCC coding involves identifying and documenting HCCs during patient encounters or hospital stays. This real-time approach ensures the capture of all relevant diagnoses and maximizes the accuracy of risk adjustment and subsequent reimbursement.
Prospective HCC Coding
Prospective HCC coding involves predicting and assigning HCCs based on historical health data and pre-existing conditions. This coding method is commonly used in insurance settings, where the risk of individuals is assessed before providing coverage or calculating premiums.
Retrospective HCC Coding
Retrospective HCC coding focuses on reviewing past medical records and claims data to identify any missed or undocumented HCCs. It allows for retrospective risk adjustment, recalculating reimbursement rates based on the newly identified conditions.
Role Of RAF In HCC Coding
HCC coding utilizes the combination of patient demographics, such as gender and age, along with the corresponding ICD-10 codes to accurately calculate the Risk Adjustment Factor (RAF). The RAF score is an essential factor in assessing patients’ financial aspects and risk-adjusted characteristics, taking into consideration variations in their performance, complexity, quality, and cost. Centers for Medicare & Medicaid Services (CMS) use the Risk-adjustment factor to determine payment by Medicare Advantage or the Department of Health & Human Services (HHS) for commercial risk adjustment. This calculation is used to determine the amount of payment allocated to health plans responsible for overseeing their members’ healthcare requirements.
HCC Coding Value
In HCC coding, the focus is always on “All conditions” of the body. If the patient has Asthma, lobular
pneumonia, and COPD, all three values will be added together to determine the patient’s score.
For healthy patients: Patients who enjoy relatively better health maintain a score
below 1000.
For less healthy patients: Patients with a health condition that is less than the
average possess an HCC
score of more than 1000.
Importance Of HCC Coding For Practitioners And ACOs
Hierarchical Condition Category (HCC) coding plays a crucial role in healthcare, specifically for practitioners and Accountable Care Organizations (ACOs).
Supporting Value-Based Care Initiatives
Value-based care is an essential focus in the modern healthcare landscape, aiming to improve patient outcomes while controlling costs because it focuses on providing rewards to physicians depending on quality rather than quantity. HCC coding is vital in supporting value-based care initiatives for both practitioners and ACOs. Accurate risk adjustment through HCC coding ensures that providers are appropriately reimbursed for their care. This, in turn, encourages practitioners to focus on preventive and coordinated care rather than unnecessary and costly interventions. ACOs, as entities responsible for managing the health of a defined population, can leverage HCC coding to measure and improve the quality of care delivered while maintaining financial sustainability.
Increased Revenue
Accurate HCC coding is vital for appropriate reimbursement in value-based care models. ACOs rely on risk-adjusted payment methodologies that consider the severity of patient conditions. Properly coding HCCs, practitioners, and ACOs can ensure they are reimbursed accurately for their care to patients with complex and costly conditions.
Maintaining Compliance
Compliance in HCC coding refers to adhering to the established guidelines, regulations, and coding principles set forth by relevant authorities such as the Centers for Medicare and Medicaid Services (CMS) in the United States.
Quality Measures
Accurate HCC coding contributes to improved quality of care and patient outcomes. Proper documentation and coding of medical conditions facilitate better communication among healthcare providers, enhance care coordination, and support evidence-based decision-making.
Tips For HCC success
Conducting Regular Training for Providers and Coders
Regular training and learning of the staff involved in HCC play a significant role because constant learning will make them updated on the new changes and guidelines.
Reviewing And Updating Documentation Processes
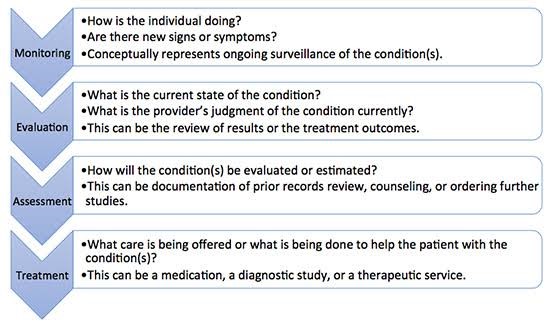
Successful reviewing of documentation requires healthcare providers to follow the MEAT rule.
M stands for “Monitor signs and symptoms.”
E stands for “Evaluation.”
A Stands for “assessing the patient records, patient education, etc.”
T stands for “treatment provided.”
Identify Potential Areas For Improvement
Here are some potential areas for improvement in HCC coding:
- Documentation specificity and clarity
- Compliance
- Coding accuracy
- The capture of the chronic condition
- Evaluation of technology
Implement Technology
Here’s how technology can assist in improving HCC coding:
Electronic Health Record (EHR) Systems: An EHR system streamlines the coding process
by allowing easy
access to patient information, lab results, diagnostic reports, and previous documentation. EHRs often
come with coding tools and prompts that can help ensure accurate code selection and documentation.
Computer-Assisted Coding (CAC): CAC software uses natural language processing and
machine learning
algorithms to analyze clinical documentation and suggest appropriate codes. CAC can help identify
potential HCC codes, flag missing documentation, and enhance coding accuracy. It speeds up the coding
process and reduces the chances of coding errors.
Encoder Software: Encoder software provides up-to-date code sets, official coding
guidelines, and
reference materials. It assists in code assignment by suggesting appropriate codes based on
documentation.
Scrutiny
Scrutiny is indeed an essential aspect of HCC coding success. To ensure accurate HCC coding and maximize reimbursement, applying scrupulous scrutiny when reviewing patient documentation and assigning appropriate HCC codes is crucial.
Harness the power of hierarchical condition category coding with MedsIT Nexus medical coding services!
Introducing MedsIT Nexus , your ultimate partner in unlocking the power of Hierarchical Condition Category (HCC) coding! MedsIT Nexus medical coding services are meticulously tailored to optimize accuracy, efficiency, and revenue potential for healthcare providers like never before. With our team of highly skilled and certified coders, we go beyond the conventional coding approach, delving deep into the intricacies of HCC coding to capture every relevant detail and ensure maximum reimbursement. Our innovative technology solutions and expert knowledge enable us to navigate the complex hierarchy of medical conditions, identify risk scores, and facilitate seamless documentation. Trust us to revolutionize your coding experience, streamline operations, and pave the way to unparalleled financial success in the evolving healthcare landscape.
Dr. Sana Pervez, Pharm.D, CCS, CPC -
Clinical Compliance Advisor at MedsIT Nexus
Responsible for Medical and compliance review of all healthcare RCM and billing content before publication.